Tibialis Posterior Tendon DysfunctionTibialis Posterior Tendon Dysfunction (TPTD) / Tendonitis / TendinopathyThe tibialis posterior tendon runs around behind your inside ankle bone (medial malleolus) and it is arguably the second most important tendon coming from your leg that attaches onto your foot. Only the achilles tendon is more important for normal foot function. The tibialis posterior tendon acts to support the arch of your foot and in doing so allows the achilles tendon to lift the heel off the ground.
| 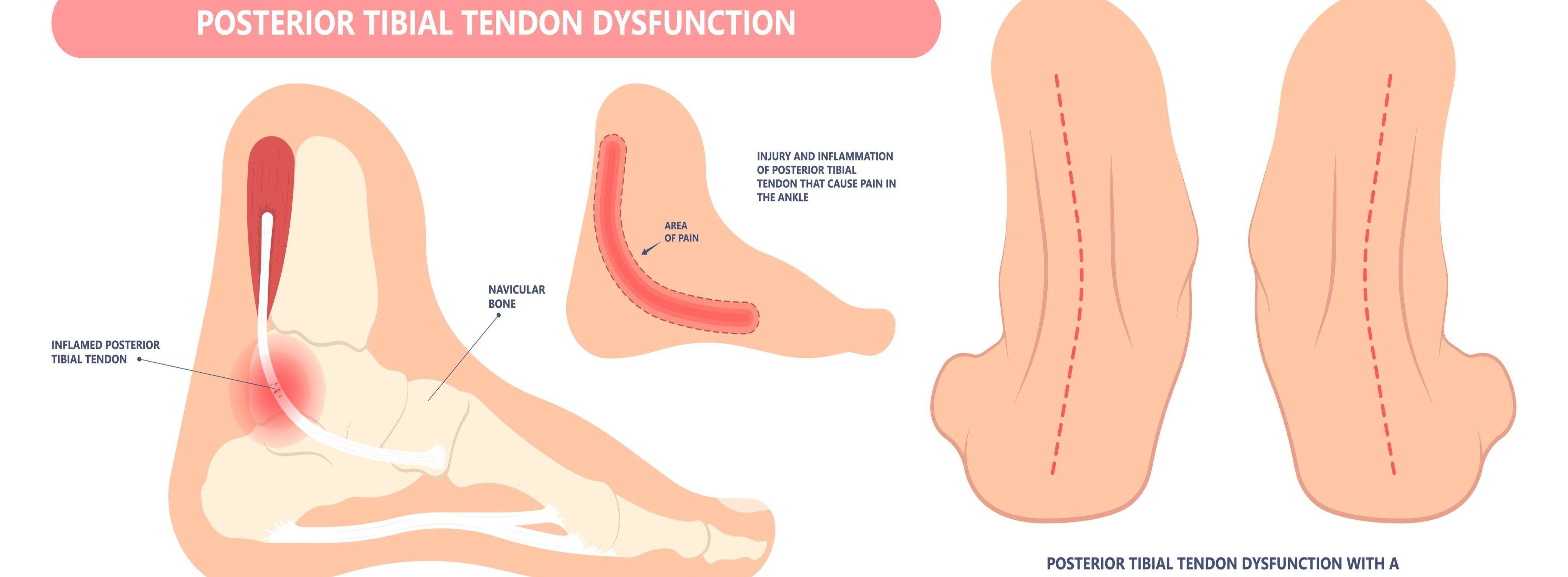 |
 | Overuse is often the cause of tibialis posterior tendinopathy (tendonitis) which, if left untreated, can lead to tibialis posterior tendon dysfunction and results in degenerative changes (splits and tears) of the tendon and progressive flattening of the foot. TPTD can also occur after a minor trip or stumble that results in damage to the tendon. The symptoms can include swelling and pain below your inside ankle bone, flattening of the arch, pain with pushing off your foot, and an inward rolling of the ankle. If left undiagnosed and or incorrectly treatment TDTD can progress to further flattening of the foot and unfortunately severe foot arthritis which then presents as pain on the outside of the foot below the lateral ankle bone. |
The correct diagnosis of the level (stage) of the dysfunction is critical to avoid the further progression of the dysfunction. This diagnosis of the stage is based on the combination of the clinical assessment of your foot and ankle combined with an Ultrasound and or an MRI depending on the clinical evaluation.
TPTD can be progressive in nature and hence early diagnosis and treatment is strongly advised. If treated early enough before the tendinopathy has progressed to TPTD your symptoms may resolve with conservative (non-surgical treatment). Untreated TPTD can lead to a flat foot, painful arthritis and increasing limitations on walking and weightbearing activities.
Conservative Treatment options may include:
- Cam Walkers (Moon Boot)
- Foot orthotics
- Ritchie bracing
- Shoe Modifications
- Home exercise program
Sometimes the best option to arrest the progression of TPTD might include surgery ranging from tendon repair with arch reconstruction to arch fusion. Surgery should always be supplemented with shoe modifications and orthotics.
All patients that have been diagnosed with TPTD must be reviewed every 12-18 months without fail to ensure the condition is not progressing unchecked.